Introduction: The Promise and Problem of Living Drugs
In the fight against cancer, one of the most revolutionary ideas has been to use the body’s own immune cells as a “living drug.” By engineering cells like CAR-T cells to recognize and attack tumors, scientists have created powerful, personalized therapies. This approach has saved lives but comes with significant challenges. Creating these custom cells from a patient’s own blood can take several weeks—a dangerously long time for someone with an aggressive disease.
The logical alternative is to use pre-made cells from a healthy donor. The problem? A patient’s immune system is designed to recognize and destroy anything it sees as “foreign,” including these life-saving therapeutic cells. This leads to swift rejection, rendering the treatment ineffective.
Now, a team of researchers at MIT and Harvard has developed a brilliant solution to this problem. They have designed a single, elegant piece of genetic engineering that cloaks these cancer-fighting cells, making them invisible to the patient’s immune system while simultaneously upgrading their potency, paving the way for a new generation of powerful, off-the-shelf cancer treatments.
A Multi-Tool for Cellular Engineering
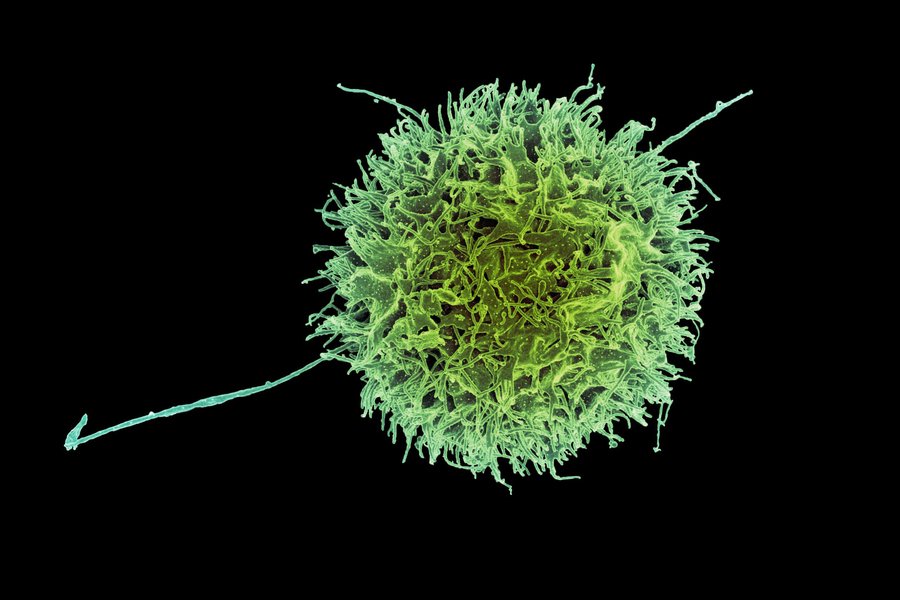
The key to making donor cells work is to hide them from the host’s immune system. Researchers focused on a type of immune cell known as a “natural killer” (NK) cell, which is adept at finding and destroying cancer cells. Their main obstacle was the HLA class 1 proteins on the cell surface, which act like identification tags. If a host’s T-cells don’t recognize these tags as “self,” they launch an attack.
To solve this, the team designed a single piece of DNA—a “construct”—that carries multiple genetic instructions. One of these instructions engineers the CAR-NK cells to permanently produce a sequence of siRNA (short interfering RNA) that interferes with the genes for HLA class 1 proteins. This built-in factory effectively removes the cell’s identification tags, allowing it to slip past the body’s defenses.
But this construct did more than just provide a disguise. The researchers also packaged it with the gene for a second protein—either PD-L1 or single-chain HLA-E (SCE)—that makes the NK cells even more effective by boosting the genes involved in killing cancer cells. This single, multi-functional construct turns a donor cell into an invisible, more potent, and safer therapeutic in one efficient step.
“This enables us to do one-step engineering of CAR-NK cells that can avoid rejection by host T cells and other immune cells. And, they kill cancer cells better and they’re safer.” — Jianzhu Chen, an MIT professor of biology, a member of the Koch Institute for Integrative Cancer Research, and one of the senior authors of the study
The Dawn of “Off-the-Shelf” Cancer Therapy
This elegant, all-in-one engineering approach opens the door to creating “off-the-shelf” cellular therapies that are ready whenever a patient needs them. The traditional method of creating personalized CAR-T or CAR-NK cells involves a lengthy process of isolating, engineering, and growing a patient’s own cells. Not only is this multi-week wait a critical period where the disease can progress, but cells derived from a sick patient “may not be as viable as cells that came from a healthy person.”
Because these new engineered CAR-NK cells can evade rejection, they can be created from healthy donor cells, grown in large quantities, and stored for immediate use. This transforms the treatment paradigm from a bespoke, time-consuming process to a readily available therapy. The implication is massive: patients could receive a powerful, living drug as soon as they are diagnosed, drastically improving the accessibility and speed of cancer treatment.
A Safer and More Potent Weapon
Beyond being faster and more accessible, this new approach also creates a therapy that is both safer and more effective. In a study using mice with human-like immune systems, the results were striking. The engineered “stealth” CAR-NK cells survived for at least three weeks and were able to nearly eliminate the cancer. In contrast, standard CAR-NK cells were quickly destroyed by the host immune system, and the cancer spread unchecked.
Critically, this new method also addresses a major safety concern with immunotherapy. The engineered cells were much less likely to cause “cytokine release syndrome,” a common and potentially life-threatening side effect where the immune system overreacts. This improved safety and efficacy profile means the core engineering “construct” could potentially be added to other CAR-NK therapies currently in development, amplifying its impact across different cancer treatments.
Conclusion: A New Blueprint for Cellular Medicine
By programming therapeutic cells to be “invisible” to the host immune system, researchers have overcome a fundamental barrier in cellular medicine. This breakthrough creates a path toward treatments that are not only more potent but also faster, safer, and accessible to more people.
The potential of this technology extends beyond cancer. Researchers are already exploring how these immune-evasive cells could be used to treat autoimmune disorders like lupus, where the immune system mistakenly attacks the body’s own healthy tissues. This work provides a new blueprint for the future of medicine.
As we learn to program our cells with this level of precision, what does the future of medicine look like when a cure might one day come not from a bottle, but from a bag of pre-made, intelligent cells?
Source: MIT News